Antimicrobial resistance (AMR) is often seen as complex and technical, inaccessible to those without medical expertise and background in public health. For the last year, here at the Global Partnership we’ve been working with the Africa’s Voices Foundation to dispel this, engaging with people and communities to learn more about what the challenges of AMR look like day-to-day, and better understand what people know about the misuse of antimicrobials.
In this work, we’ve spoken to everyone, from mothers to health care workers to policymakers and veterinarians about their understanding of AMR and what needs to be done to tackle AMR. One story shared by Mary, who works as a nurse in Kilifi County, has stayed with me in particular. An HIV-positive couple in rural Kenya would regularly attend a local health facility to receive their antiretroviral prescription. Mary realized that the wife was not going to the health facility regularly to get more medication, instead she was innocently taking her husband’s medication when she ran out. This was convenient for her, but she was at risk of becoming resistant to the medication due to misuse.
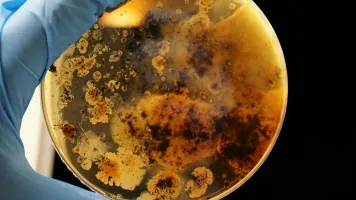
This is one dimension of what AMR looks like day to day. Sadly, there are more stories around the misuse of antibiotics than we will ever actually hear or document. Misuse of antimicrobials is all too common, and drug resistance is a growing threat here in Kenya, and globally. Yet, we are not able to communicate the urgency of AMR because we still do not have a very clear picture of its magnitude and consequences. We still struggle to effectively measure it. The existing surveillance data is sketchy, despite progress seen through the World Health Organization’s Global Antimicrobial Resistance and Use Surveillance System in 2015. Surveillance data alone is not sufficient to understand and tackle AMR. We need complementary non-traditional data sources to close the data gaps, gather more nuanced insights on the level of awareness around AMR, and gain greater clarity on what drives behavior around using (and misusing) antimicrobials.
Here, citizen-generated data (CGD) is crucial. By engaging people on the topic—and in the process generating data with them—people can understand the consequences of AMR and take action to fight it.
This week, we are publishing the findings from our year-long study using citizen-generated data to address AMR in Kenya. In three counties—Kiambu, Kilifi, and Bungoma—we hosted 10 weeks of interactive radio shows. Alongside the radio shows and in-person community listening groups, SMSs received throughout the shows helped us paint a picture of Kenyans’ understanding and behaviors surrounding the use of antibiotics.
Here are three insights on AMR we’ve drawn from engaging with people and communities across Kenya:
1. AMR is a systemic issue that requires a holistic approach.
The challenges of access and availability of health facilities, as well as the high costs of seeking medical care, lead to poor health-seeking practices, which exacerbate AMR. This cycle is further reinforced by inadequate and under-resourced health facilities, leading to long hospital queues and not enough time for health workers to engage meaningfully with citizens on AMR. In addition, although regulations for medications exist, the level of awareness and enforcement is low. Improving health systems is essential, and an important part of this is improving communication for healthcare providers and for patients.
2. Improving community awareness of antibiotics is central to moving the needle on the fight against AMR.
Our insights point to poor, and even risky, health-seeking behaviors for antibiotics among citizens in Kenya. Most patients seek care too late, when other means, such as self-treatment, fail or when antibiotics may not be needed. Other times people don’t visit health facilities, preferring to buy antimicrobials over the counter or rely on traditional medicine instead.
Often, people misuse antimicrobials due to a lack of knowledge of the proper use, the risks and consequences, as is evident in the story above of a woman taking her husband’s antiretrovirals.
The findings from this study demonstrate that there is an identifiable benefit to public engagement on AMR in Kenya. Even within the span of 10 weeks, we measured an increase in interest and knowledge on AMR. This interest indicates that targeted and consistent public engagement on AMR can reduce knowledge gaps and ultimately influence behavior change to address AMR.
3. Stepping up in the fight against AMR requires greater investment in healthcare.
Most people obtain information on antimicrobials or on AMR through interactions with health care workers when they seek medical care or during the process of receiving guidance on how to take medication.
But, currently health systems in Kenya do not give people enough time to have quality interactions. Instead, health care workers are forced to make trade-offs between meaningful engagement with patients and attending to long queues. Conversely, some citizens demand medication in a specific form—for example, an injection—and when they don’t receive the requested treatment, they get frustrated and question the competence of the care providers.
Greater investment of time and resources is essential. Find out more about this, and other priorities for tackling AMR, in the video below.
Our findings paint a clear picture of the roles that everyone in Kenya, from people and their communities to health care workers to policymakers, can play in tackling AMR. Everyday insights are critical in guiding the Kenyan government in decision-making, as well as the health decisions we make as individuals. Data, both quantitative and qualitative, must be at the center.
Read the interactive report here.
This blog is part of a series on citizen-generated data and antimicrobial resistance in Kenya. Find out more about using citizen-generated data in this guest blog from Africa’s Voices Foundation.